Tackling cancer: the immunotherapy revolution
The survival rate and quality of life of patients have increased dramatically in the last decade and cancer spending has tripled.


BarcelonaEvery week, new scientific literature on cancer is published, leaving patients and their families dreaming of possible care. But the revolution against this disease began more than a decade ago, with the approval of the first immunotherapies, which stimulate our body's defenses to attack malignant cells. Patient survival has changed radically thanks to these drugs, which have demonstrated success that was unthinkable a few years ago with traditional treatments. There is still a long way to go: some patients respond very well to treatment, but others relapse over the years, and some with very aggressive tumors continue to have a very poor prognosis. However, the emergence of immunotherapy has marked a paradigm shift in the fight against cancer, and experts maintain that we must continue exploring new forms of treatment to fully exploit its potential.
"Immunotherapy has shown that very long survival times can be achieved in most tumors. We are now seeing cases with metastases that survive five, seven, or ten years, and that was previously unthinkable," explains Ernest Nadal, research director at the Catalan Institute of Oncology (ICO). To understand how these drugs work, it is necessary to understand the mechanisms that tumors use to escape our immune system. Cancer cells take advantage of a protein in white blood cells (those responsible for protecting us from external threats) to camouflage themselves, so in the eyes of our defenses they appear to be healthy cells and the tumor has room to continue growing and put our survival at risk.
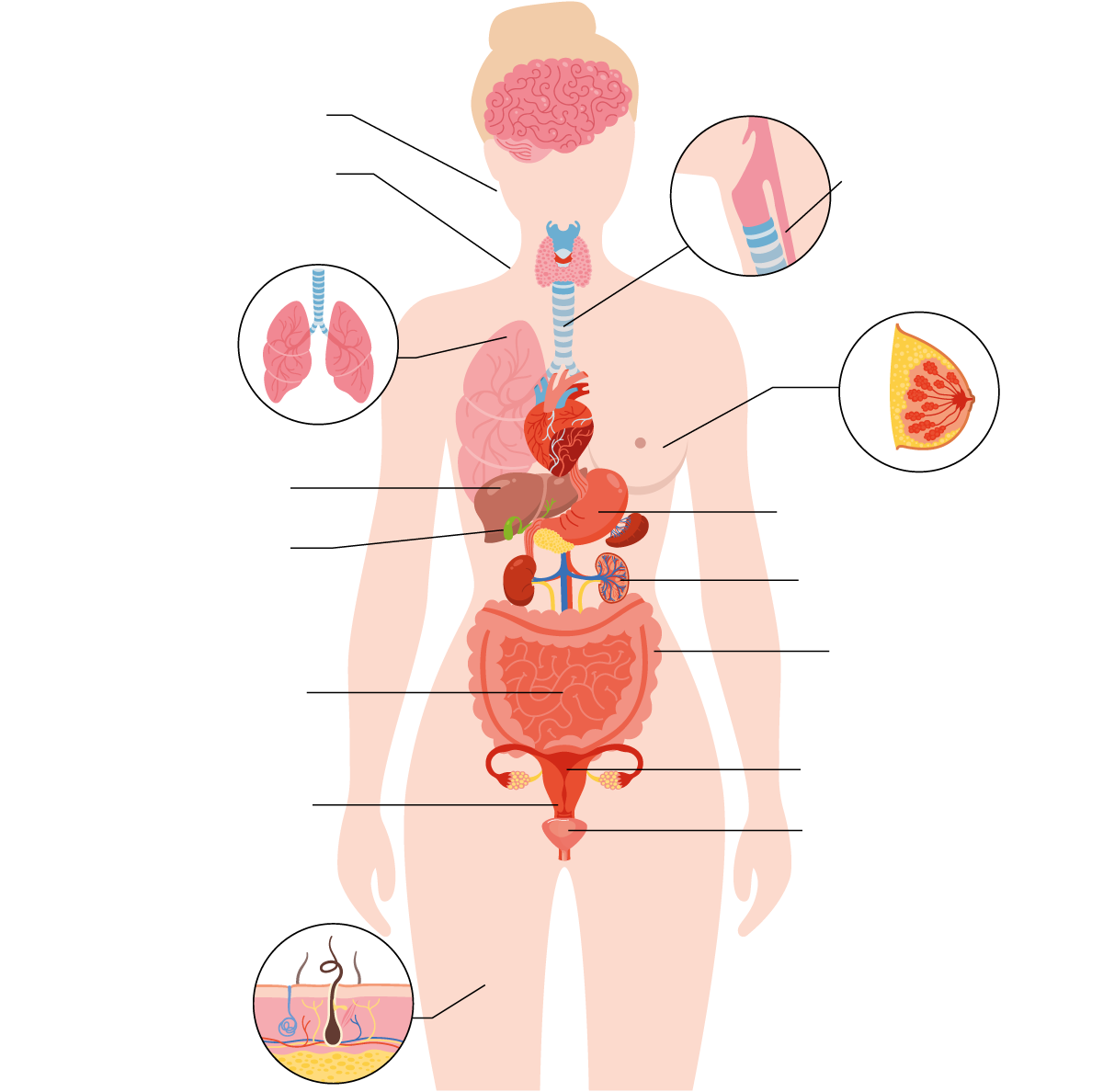
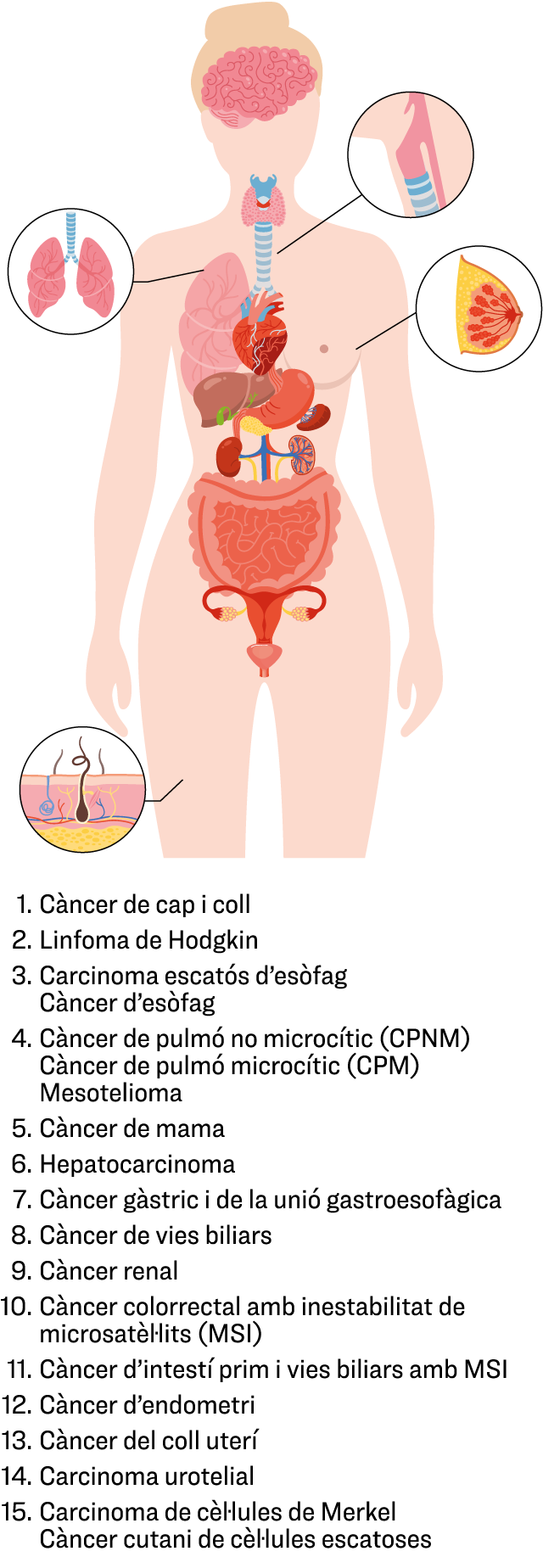
Immunotherapy acts on this escape mechanism used by the tumor and unmasks it so that immune cells recognize and attack it. Over the last decade, new immunotherapies have been incorporated into the public health portfolio, and there are currently 68 available to treat up to eighteen different types of cancer, according to the Ministry of Health. Thanks to these drugs, many cancer patients have overcome unthinkable battles, improved prognoses, and, in some cases, the disease has become chronic for life.
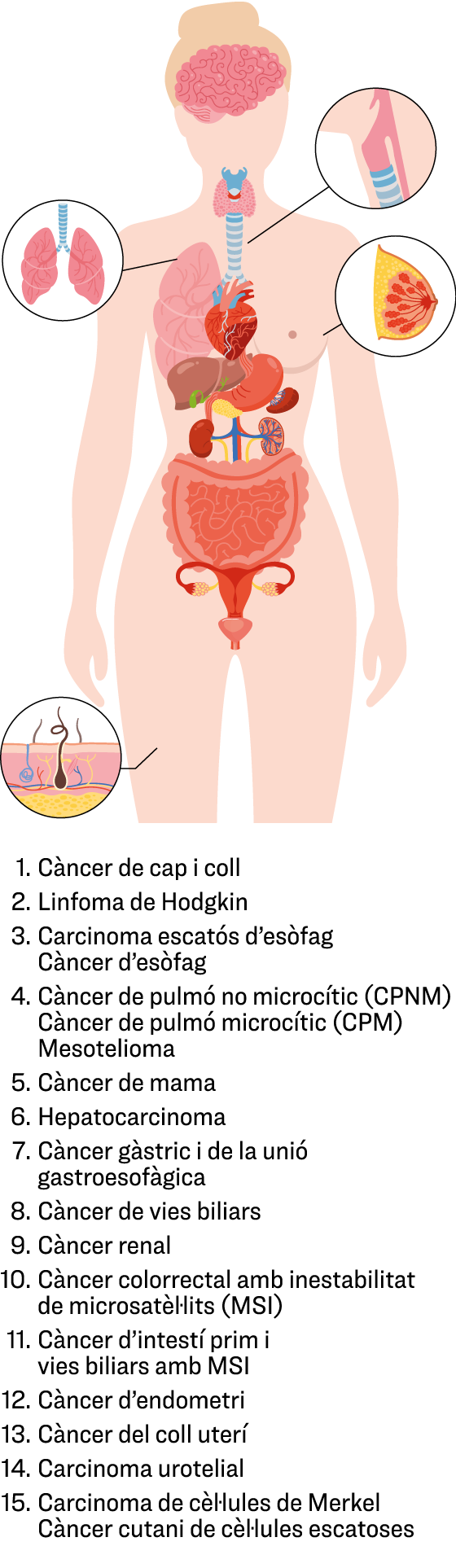
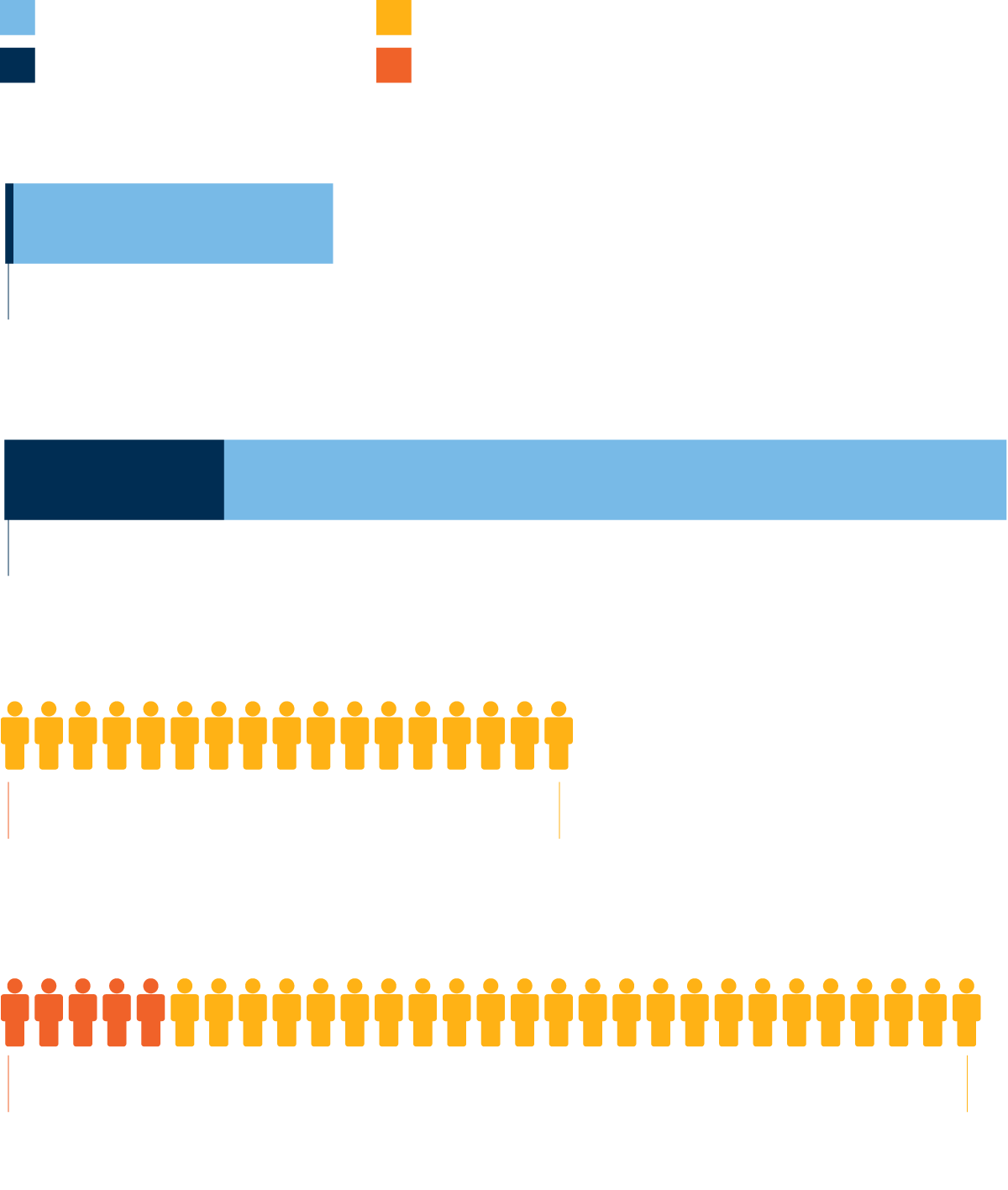
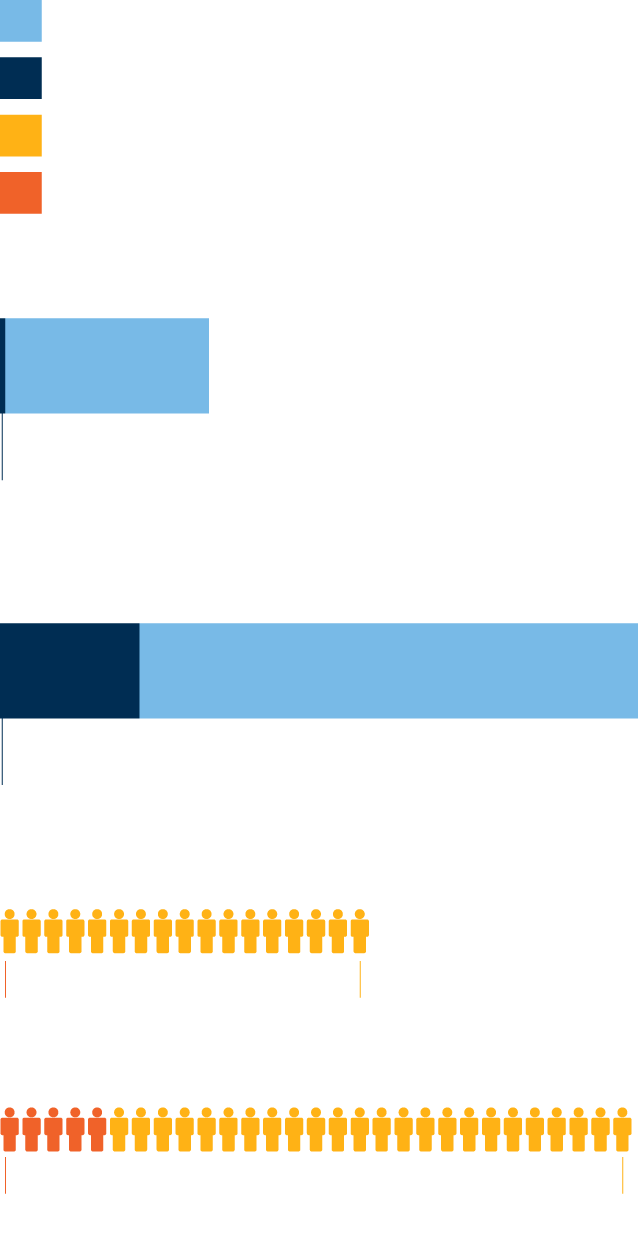
In fact, this revolution is clearly reflected in the number of patients receiving treatment. For example, in 2015, only 73 patients in Catalonia were receiving immunotherapy, representing 0.36% of the total number of cancer patients in our country. Last year, however, 6,387 people received immunotherapy in Catalan healthcare centers, representing 17.81% of the total number of patients. The number of patients receiving immunotherapy has grown exponentially over the last ten years, and the upward trend continues. Provisional data for 2025 indicates that the figures for last year have almost surpassed those for the previous year, and nearly one in five cancer patients in Catalonia is receiving some form of immunotherapy.
Combine treatments
Combining immunotherapy with other treatments, such as chemotherapy or radiotherapy, is another key to fighting cancer. Some tumors respond very well to immunotherapy alone, and the prognosis for patients is generally good, such as melanoma. However, others are more complicated, and immunotherapies have not yet completely replaced older treatments. Instead, a combined approach is used to achieve a better response. This is the case with lung cancer, for example, which is very aggressive. Immunotherapy alone is not enough, and patients also receive chemotherapy and radiotherapy before the drug.
In other cases, immunotherapy is applied first, followed by surgery to remove the tumor, which is weaker thanks to the previous treatment. This improves the prognosis for patients after surgery. However, there are an increasing number of diseases for which immunotherapy is becoming the standard treatment. In fact, the scientific community's efforts are focused on moving the use of these drugs to the earliest stages of cancer, since with the passage of time, tumors have a greater ability to evade our defenses and progress, and some have already been approved for initial stages, according to Nadal.
The expert believes that we should not slack off and that we must continue researching these treatments to develop more and better drugs, especially for tumors with a worse prognosis that still have no therapeutic alternatives. "We are much better off than ten years ago, of course, but we shouldn't be satisfied with what we have; we still have a long way to go," the researcher argues. For example, he explains that many pharmaceutical companies have conducted similar research to be able to patent their own treatment, but, on the other hand, there are rarer tumors that companies have not researched as much, and this is where he believes research centers and universities should focus on generating new evidence.
Three times the spending in a decade
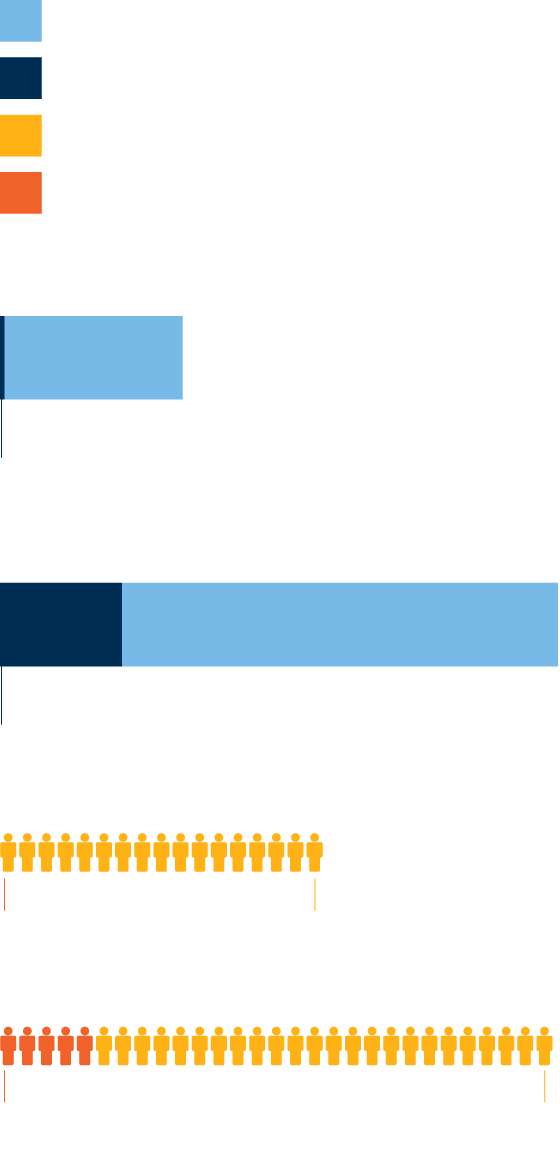
Another good example of the impact that the incorporation of these treatments has had on the public health services portfolio can be found in the budget of the Department of Health. When a previously unheard-of therapy is added, it must be taken into account that not only is a new treatment being purchased, but also that centers must be scaled, spaces must be provided, professionals must be trained, new ones must be hired, and a whole series of changes must be implemented progressively so as not to shake the fragile economy of the health system. And this is what has happened with the introduction of these drugs. In the last decade, cancer spending in Catalonia has tripled, and a large portion of these resources are allocated to these treatments: one in every five euros of cancer spending is now for immunotherapies.
According to data from the Department of Health, in 2015, investment in these drugs was close to €3 million and represented 2.43% of total cancer spending, while last year the cost allocated was almost €80 million—27 times more—and represented 21.91% of cancer spending. With this year's provisional figures, investment in immunotherapy is already a percentage higher than last year, meaning it accounts for a larger share of the total resources allocated to the fight against cancer in Catalonia. Experts also predict that this will increase, both due to the incorporation of new drugs into the public health system and the increase in the number of patients requiring cancer treatment, as cancer cases are set to rise in the coming years.
Adverse effects
Aggressive tumors with a poorer prognosis and no therapeutic alternatives are one of the outstanding tasks for immunotherapies, but there are other aspects of these drugs that need to be improved. Since they stimulate our immune system and it is our defenses that attack the tumor, they have fewer adverse effects than traditional treatments, such as chemotherapy or radiotherapy, which are more aggressive on our body. However, Nadal warns that they also have side effects that should be known before starting a treatment of this nature.
Stimulating the body's defenses can cause a "certain loss of control of the immune system," and patients may experience inflammation of the thyroid or colon and even develop an immune disease. The expert assures that the professionals who administer these drugs are very attentive to possible adverse effects in order to act quickly, which means that most disorders caused by immunotherapy are easily controlled and "are rarely fatal." Unlike chemotherapy, which causes nausea, hair loss, vomiting, and a generalized decrease in immune system, these treatments primarily affect the skin, liver, thyroid, and joints, and in some cases even cause arthritis in patients. Sometimes the inflammation can affect the heart, brain, kidneys, or lungs, where the risk of complications is higher, but Nadal assures that these conditions are very rare and, in general, control is good.
The hopeful path that immunotherapy has opened for cancer patients must continue and bring even better news in the future, especially in places where there is still no therapeutic alternative. Much research is focused on this: finding new treatments that result in increasingly higher survival rates and quality of life for patients, and developing new strategies that combine immunotherapy with more effective treatments and drugs to increasingly increase the number of people with cancer who are cured or, at least, achieve chronic disease.